When most people think of dental implants, the focus tends to be on the implant post or the crown that replaces a missing tooth. But there’s something even more important than those components: your gum health. Healthy gums are the foundation upon which the success of dental implants rests. Without strong, disease‑free gum tissue, even the best implant can fail — and no one wants that after investing time, money, and hope into a new smile.
In this article, we’ll explain why gum health matters, how it affects implant success, and what periodontal therapy (gum treatment) does to prepare your mouth for a lifetime of confident chewing and smiling.
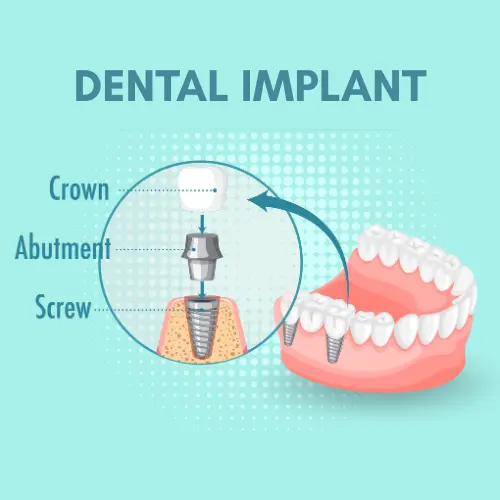
Dental Implants — More Than Just a Replacement Tooth
Dental implants are titanium posts that act like artificial tooth roots, anchoring a crown, bridge, or denture in place. They fuse with your jawbone in a process called osseointegration, forming a secure, long‑lasting foundation for artificial teeth.
However, implants rely on more than just bone — they also rely on healthy gum tissue. The gums serve as a protective seal around the implant. If this seal is weak or infected, bacteria can enter, inflammation can occur, and the entire implant can be compromised. This means that gum health before dental implants isn’t optional — it’s essential to long‑term success.
What Are Gum Problems — And Why They Matter
When your gums are unhealthy, it’s usually because of gum disease — a progressive infection caused by plaque and bacteria. Gum disease begins as gingivitis (inflamed, tender gums) and can progress to periodontitis, where the infection spreads deeper, damaging the tissues and bone that support teeth (and future implants).
Here’s what can happen if gum disease isn’t addressed before implant placement:
• Impaired Osseointegration
Inflamed gums interfere with your body’s ability to heal and integrate the implant into the bone. Successful osseointegration is key to implant stability.
• Higher Infection Risk
Periodontal bacteria don’t disappear when teeth are missing — they can invade the tissues around implants, causing peri‑implantitis, a destructive inflammation of the gums and bone.
• Bone Loss Around Implants
If gum disease progresses, it accelerates bone loss. Bone supports the implant, so losing bone weakens the entire structure.
• Poor Aesthetics
Gum recession can expose implant components or make the gumline look uneven, jeopardizing the natural look of your smile.
Peri‑Implantitis — The “Gum Disease” of Implants
Even after an implant is successfully placed, unhealthy gum tissue can cause serious problems. The bacterial infection that affects implants is called peri‑implantitis. It starts with inflammation of the gums around the implant (similar to gingivitis) and, if left untreated, destroys bone and soft tissue around the implant.
Signs of peri‑implantitis include:
- Red, swollen gums around the implant
- Bleeding while brushing or flossing
- Pus formation
- Loosening of the implant
Because implants don’t have periodontal ligaments like natural teeth, the implants are more susceptible to bacterial invasion when gum health is compromised.
Periodontal Therapy — Preparing Your Gums for Implants
Treating gum disease before implant placement is not just beneficial — it’s a standard of care recommended by dental professionals. The goal of periodontal therapy is to eliminate infection, restore healthy gum tissue, and create a stable environment where implants can thrive.
Here’s how periodontal therapy prepares your mouth:
• Comprehensive Gum Assessment
Your dentist or periodontist measures gum pockets, checks for bleeding, and assesses bone levels. This creates a roadmap for treatment and ensures your gums are truly ready. Professional tools like periodontal charting help with accurate diagnosis.
• Scaling and Root Planing (Deep Cleaning)
This non‑surgical treatment removes plaque and tartar from below the gum line, helping reduce inflammation and allowing the gums to reattach to the tooth or implant site.
• Periodontal Surgery or Pocket Reduction
If deep periodontal pockets persist, surgery may be needed to clean infected areas thoroughly and reduce pocket depth.
• Gum Grafting
When gum tissue is thin or receded, grafting can strengthen the gum around a future implant site, reducing the risk of recession later. This creates a healthier, more protective gum contour around the implant.
• Bone Grafting (when needed)
If bone loss has occurred due to gum disease, bone grafting rebuilds support for the implant, creating a stronger foundation.
• Healing and Re‑Evaluation
Only once gum inflammation is controlled and tissue is stable does the implant surgery proceed — a staged approach proven to improve outcomes.

The Benefits of Treating Gum Disease Before Implants
Addressing gum health before implant surgery offers a range of benefits that go beyond just implant stability:
• Stronger Implant Integration
Healthy gums help your body focus on fusing the implant with bone, rather than fighting infection.
• Reduced Risk of Peri‑Implantitis
By eliminating gum inflammation first, you lower the chance that infection will affect your new implant.
• Better Appearance and Gum Contours
Well‑managed gums provide a natural frame around your implant, enhancing aesthetics.
• Easier Long‑Term Maintenance
Healthy gums are easier to clean and care for, reducing long‑term risk of biological complications.
• Higher Overall Success Rates
Data from multiple dental sources show that patients with healthy gums have significantly higher implant success and longevity compared to those with untreated periodontal issues.
What You Can Do to Improve Gum Health
Improving gum health doesn’t stop at the dentist’s office — it must continue at home:
Daily Hygiene Habits
- Brush twice daily with a soft toothbrush
- Use interdental brushes or floss to clean between teeth and around implant sites (interdental cleaning helps prevent gum disease)
Lifestyle Adjustments
- Quit smoking (smoking slows healing and increases the risk of infection)
- Manage conditions like diabetes that can compromise healing
Regular Professional Care
- Dental cleanings every 3–6 months
- Periodontal maintenance checks
These habits help create and maintain the gum health needed for implants to last for decades.
Signs You Should See Your Dentist Before Implant Surgery
Not all gum disease is obvious. Seeing a dental professional early helps catch problems before they escalate. Schedule an evaluation if you notice:
- Bleeding while brushing or flossing
- Red, swollen or tender gums
- Gums pulling away from teeth
- Bad breath that won’t go away
- Pain or discomfort around teeth or gums
Early treatment not only preserves gum health, but also ensures a smoother, safer implant journey.
Life After Implants — More Gum Care
Even after your dental implants are placed, gum health remains vital. Implants can develop peri‑implantitis — an inflammation similar to gum disease — if plaque and bacteria accumulate around the base.
To protect your investment:
- Maintain excellent oral hygiene every day
- Keep regular dental appointments
- Watch for any signs of inflammation around implants
- Report any changes (bleeding, sensitivity, swelling) to your dentist promptly
Ongoing care ensures your implants stay healthy and functioning for many years.
Frequently Asked Questions About Gum Health & Dental Implants
A: Gum disease must usually be treated before placing dental implants. Active infection can interfere with healing and increase the risk of implant failure. Periodontal therapy helps create a healthy, stable foundation for successful implant placement.
A: Healthy gums form a protective seal around the implant, reducing bacterial entry and inflammation. Strong, disease-free gums support healing and significantly improve long-term implant success.
A: Periodontal therapy treats gum infection and inflammation through deep cleaning, gum treatment, or surgical care if needed. It prepares the gums and supporting bone to safely support dental implants.
A: Untreated gum disease can lead to implant infection, bone loss, peri-implantitis, and even implant failure. Treating gum disease first greatly reduces these risks.
A: Daily brushing and flossing, regular dental visits, professional cleanings, and avoiding smoking are essential. Ongoing gum care helps protect implants and ensures long-term success.
Conclusion — Healthy Gums Build Strong Smiles
Strong, disease‑free gums are the unsung heroes of dental implant success. Before any implant surgery, your gums must be evaluated, treated, and stabilized through periodontal therapy so that your body can support the new implant and protect it against bacterial invasion.
Healthy gums don’t just help implants fuse properly — they protect your investment, preserve bone, enhance aesthetics, and improve long‑term outcomes. By working with skilled dental professionals and committing to excellent oral care, you give your implants the greatest chance of lasting a lifetime.
Ready for dental implants? Start with your gum health — it’s the foundation of your smile.
References
- Dental Implant Procedures– American Academy of Periodontology
- Dental Implant Surgery– Mayo Clinic
- Periodontal (Gum) Disease– National Institute of Dental and Craniofacial Research
- Guideline on treatment of peri-implant diseases– European Federation of Periodontology
- The Importance of Gum Health in Dental Implant Success-Spring Hill Specialist Dental Centre
Please subscribe to our social channels for updates related to dental care and oral health.
Instagram: cdental2025
Facebook: CDental
YouTube: C-Dental Clinic







Leave a Reply